Infiltration vs extravasation is a critical topic in medical practice that every healthcare professional must understand. These terms describe complications that can occur during intravenous (IV) therapy, where fluids or medications inadvertently leak into surrounding tissues. Recognizing the differences between infiltration and extravasation is essential to ensure patient safety and prevent long-term complications.
Intravenous therapy is one of the most common medical procedures worldwide. However, it carries inherent risks, including infiltration and extravasation. While both involve the unintended leakage of IV fluids or medications, their implications and management differ significantly. Understanding these differences is crucial for healthcare providers to implement appropriate interventions.
This article will explore the distinctions between infiltration and extravasation, their causes, symptoms, and management strategies. By providing comprehensive insights into these complications, we aim to empower healthcare professionals and patients alike to recognize and address these issues effectively.
Read also:How Old Is Puff Daddy A Comprehensive Guide To His Life Career And Legacy
Table of Contents
- Definition of Infiltration and Extravasation
- Causes of Infiltration and Extravasation
- Symptoms and Clinical Presentation
- Diagnosis and Assessment
- Management Strategies
- Preventive Measures
- Risks and Complications
- Nursing Responsibilities
- Legal and Ethical Considerations
- Conclusion and Call to Action
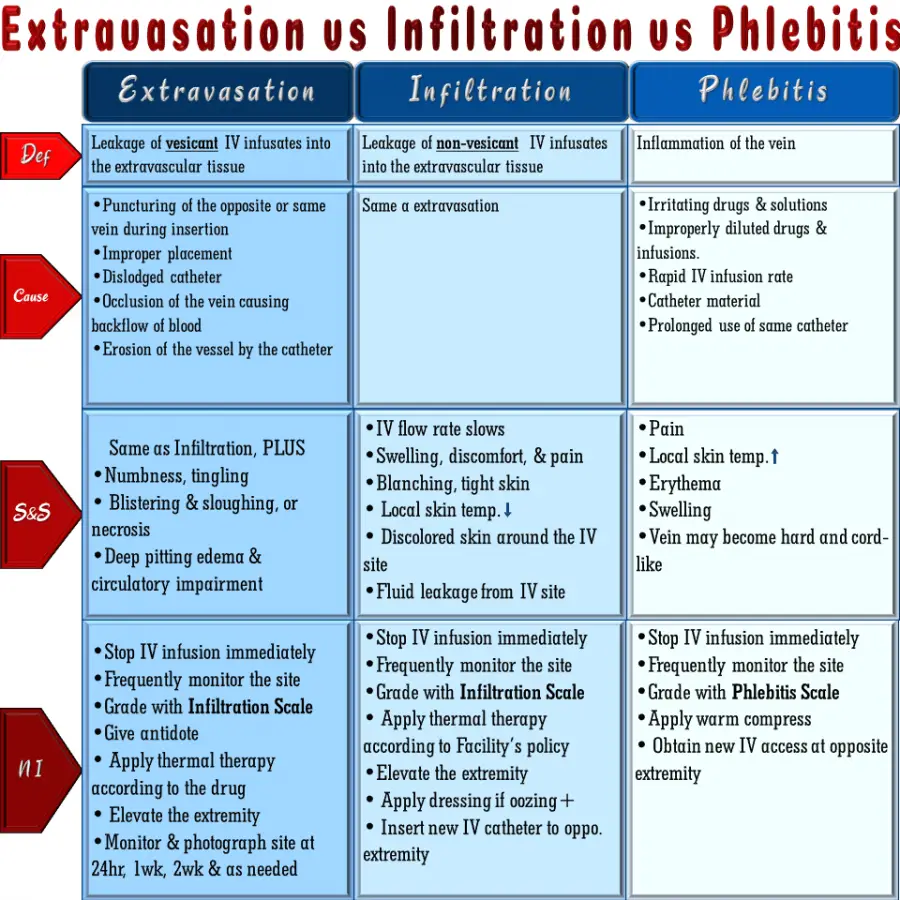
Definition of Infiltration and Extravasation
Understanding Infiltration
Infiltration occurs when non-vesicant IV fluids or medications leak into the surrounding tissues outside the vein. This complication typically happens due to improper cannula placement or dislodgement. Although infiltration is generally less severe than extravasation, it can still cause significant discomfort and tissue damage if not addressed promptly.
Defining Extravasation
Extravasation, on the other hand, involves the leakage of vesicant medications into the surrounding tissues. Vesicants are drugs that can cause tissue damage, necrosis, or even permanent injury if they escape the vascular system. Examples of vesicants include chemotherapy drugs, certain antibiotics, and hypertonic solutions. Recognizing the difference between these two conditions is vital for effective management.
Causes of Infiltration and Extravasation
Several factors contribute to the occurrence of infiltration and extravasation. Below are some common causes:
- Improper cannula placement
- Patient movement or agitation
- Use of peripheral IV lines for vesicant medications
- Underlying vascular conditions, such as vein sclerosis or fragility
- Inadequate monitoring of IV sites
Healthcare providers must remain vigilant in identifying these risk factors to minimize the likelihood of complications.
Symptoms and Clinical Presentation
Signs of Infiltration
Infiltration typically presents with the following symptoms:
- Swelling at the IV site
- Coolness or paleness of the affected area
- Slowed or stopped infusion flow
- Pain or discomfort, though often less severe than in extravasation
Extravasation Symptoms
Extravasation, being more severe, exhibits more pronounced symptoms:
Read also:Virgo And Cancer Understanding The Dynamics Of This Zodiac Compatibility
- Severe pain or burning sensation at the IV site
- Redness, warmth, and swelling
- Blistering or skin discoloration
- Potential for tissue necrosis if left untreated
Early recognition of these symptoms is crucial for timely intervention and management.
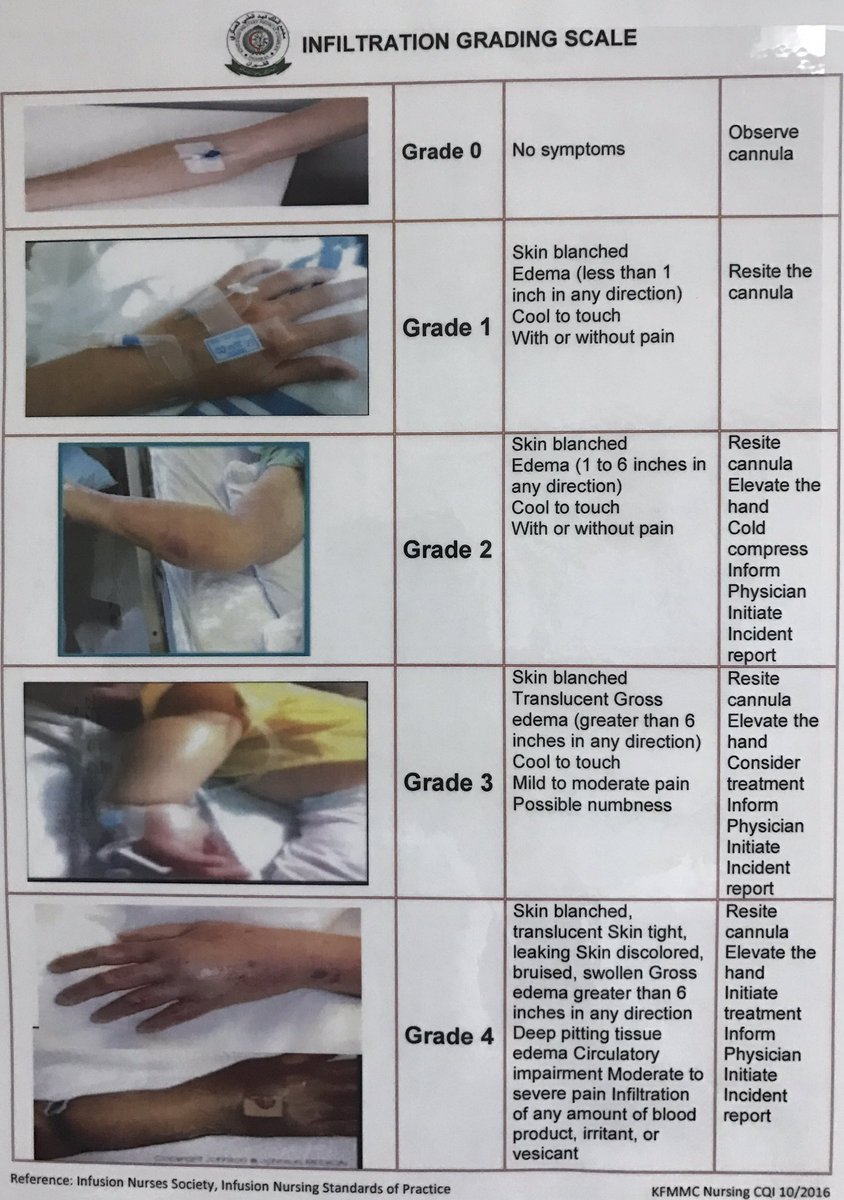
Diagnosis and Assessment
Diagnosing infiltration and extravasation requires a thorough clinical evaluation. Healthcare providers should:
- Inspect the IV site regularly for signs of swelling, redness, or discomfort
- Monitor infusion rates and ensure proper cannula placement
- Document any changes in the condition of the IV site
- Consult with pharmacists or specialists when vesicant medications are involved
In some cases, imaging studies such as ultrasound may be used to assess the extent of tissue damage.
Management Strategies
Managing Infiltration
Infiltration management typically involves:
- Discontinuing the IV infusion immediately
- Applying warm or cold compresses to reduce swelling
- Elevating the affected limb to promote fluid reabsorption
- Administering analgesics if necessary
Treating Extravasation
Extravasation requires more aggressive intervention, including:
- Stopping the infusion and disconnecting the IV line
- Aspirating the vesicant from the site, if possible
- Administering antidotes, such as hyaluronidase or dexrazoxane, depending on the medication involved
- Referring the patient to a specialist for further evaluation and treatment
Timely intervention is critical to prevent long-term complications from extravasation.
Preventive Measures
Preventing infiltration and extravasation begins with proper IV cannula placement and regular monitoring. Healthcare providers should:
- Use ultrasound guidance for difficult venous access
- Select appropriate IV sites based on patient anatomy and condition
- Secure the cannula properly to minimize movement
- Educate patients about the importance of keeping the IV site still
Implementing standardized protocols and staff training programs can further reduce the incidence of these complications.
Risks and Complications
Both infiltration and extravasation carry potential risks if not managed appropriately. Long-term complications may include:
- Chronic pain or discomfort
- Scar tissue formation
- Impaired mobility or function
- Infection or cellulitis
For extravasation, the risks are even more severe, with the potential for tissue necrosis and the need for surgical intervention. Understanding these risks underscores the importance of prompt recognition and treatment.
Nursing Responsibilities
Nurses play a pivotal role in preventing and managing infiltration and extravasation. Their responsibilities include:
- Regularly assessing IV sites for signs of complications
- Ensuring proper documentation of IV site conditions
- Providing patient education on IV care
- Collaborating with other healthcare team members for comprehensive care
Nurses should also advocate for evidence-based practices and protocols to enhance patient safety.
Legal and Ethical Considerations
Infiltration and extravasation can have legal implications if they result in harm to the patient. Healthcare providers must adhere to best practices and standards of care to minimize liability. Ethically, providers have a duty to prioritize patient safety and well-being, ensuring that all interventions are appropriate and timely.
Conclusion and Call to Action
In conclusion, understanding the differences between infiltration and extravasation is essential for healthcare professionals to ensure patient safety during IV therapy. By recognizing the causes, symptoms, and management strategies for these complications, providers can implement effective preventive measures and interventions. We encourage readers to:
- Share this article with colleagues to promote awareness
- Implement standardized protocols in their practice settings
- Engage in ongoing education and training to stay updated on best practices
Together, we can reduce the incidence of infiltration and extravasation, improving patient outcomes and enhancing the quality of care. For further reading, explore our other articles on IV therapy and patient safety.
Data Source: According to the Infusion Nurses Society (INS) and the Centers for Disease Control and Prevention (CDC), proper IV site management significantly reduces the risk of complications. These organizations provide guidelines and resources to support healthcare providers in delivering safe and effective care.